
Hormonal acne is one of the most common symptoms of PCOS (Polycystic Ovary Syndrome) which can be not only physically painful but also very mentally challenging. Since acne can seriously impact the quality of life and mental health of women with PCOS it is important to address the root cause and seek effective treatments.
After my personal experience of combating severe hormonal acne during most of my life, I understand how frustrating this condition can be (especially during adulthood). That’s why in this evidence-based article I’ll share with you everything you need to know about PCOS acne and how to get rid of it for good.
I’ll also give you some useful tips on my favorite skincare products, home remedies and supplements that helped me to heal acne and clear my skin the most.
What causes PCOS acne?
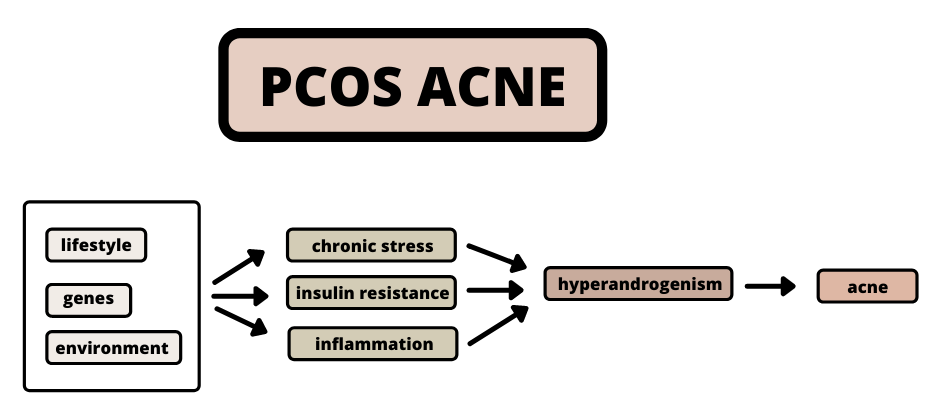
PCOS acne is predominately caused by sex hormone imbalances and excessive amounts of androgens in the blood responsible for the overproduction of sebum. Insulin resistance, chronic stress and inflammation are considered to be the main contributors to hyperandrogenism in women with PCOS.
In general, acne is developed when your skin pores get blocked by excess oil (sebum), dead skin or bacteria. There are, however, many different factors that can contribute to such consequences including:
- hormone fluctuations
- poor hygiene
- stress
- medication
- impropriate skincare products
When it comes to PCOS-induced acne, it is clear that hormone fluctuations are the main drivers of this symptom, specifically high levels of androgens in the blood (hyperandrogenism), excess cortisol and decreased levels of progesterone.
Hormone imbalance
DHT (dihydrotestosterone) is an androgenic hormone (synthesized from testosterone) that can bind to androgen receptors in the sebaceous glands. Those glands (located in your skin) can then get triggered to produce excess amounts of sebum (natural oil) that flows to your skin’s surface.
As a result, it can cause blockage in your pores, promote the growth of bacteria and contribute to inflammation and infection in your skin. Depending on your personal sensitivity, you can end up with either small whiteheads and blackheads or with painful infected cysts deep under your skin.
Cortisol (released in response to stress) is another hormone that can stimulate the production of sebum in the skin glands (similar to DHT) and contribute to clogged pores, inflammation and breakouts.
Another hormone that plays an important in your skin health is progesterone (the ‘female’ hormone). It is responsible for maintaining your skin’s hydration and elasticity which is why decreased levels of progesterone (as in women with PCOS) can make your skin more vulnerable and susceptible to acne.
Insulin resistance
If your goal is to heal acne permanently, restoring your hormonal balance should therefore be your primary focus. While PCOS is a very complex condition affected by several different factors (genetics, lifestyle, environment), insulin resistance appears to be the main contributor to hyperandrogenism in most cases.
You can find more information about the role of insulin resistance in the development and progress of PCOS here: ‘PCOS Insulin Resistance Explained & How To Reverse It’.
To put it simply, high insulin levels (hyperinsulinemia) caused by insulin resistance (your body’s inability to process insulin effectively) can signal to your ovaries to produce androgens in excessive amounts (hyperandrogenism).
Inflammation & chronic stress
Inflammation and chronic stress are other common drivers of PCOS that can affect your androgen levels and skin condition. Inflammation is not only responsible for the painful red swollen cysts underneath your skin (cystic acne) but inflammation in the body can also worsen your insulin resistance.
Additionally, chronically elevated stress levels can make your adrenals overproduce androgens and therefore contribute to hyperandrogenism through a different pathway.
Does PCOS acne ever go away?
PCOS acne is completely reversible and will go away in most women with PCOS once they address the root cause of their condition, make relevant changes and balance their hormones. However, it is a very slow process that can take up anywhere between a few weeks to several months or years.
You should keep in mind that your skin goes through natural cycles of replacing your dead skin cells with healthy ones after a certain period of time. This process usually takes between 4-6 weeks depending on your age (the older you get the longer it takes).
It is therefore important to be patient and give your body enough time to recover after adapting new treatment strategies. Occasional breakouts (especially prior to your periods) are also completely normal as your body experiences natural fluctuations in your hormones. PCOS acne is, however, very different and should be recognized.
What does PCOS acne look like?
PCOS acne can be described as large, red and deeply rooted breakouts that tend to flare on the lower face. The spots are usually painful and more difficult to heal in comparison to regular breakouts. However, the severity and location of PCOS-induced acne can largely differ between individuals.
PCOS acne location:
- Face
- Jawline
- Chin
- Neck
- Chest
- Upper back
Does everyone with PCOS get acne?
Despite the fact that acne is one of the most common symptoms of PCOS, it doesn’t occur in all individuals with this condition. It is estimated that about 1 in 3 women with PCOS suffer from acne and skin-related problems. However, PCOS is considered the leading cause of adult acne in women over 25.
Bear in mind that PCOS is a multifactorial condition and that its symptoms can greatly vary between individuals. Additionally, there might be some other underlying causes of hyperandrogenism and poor skin health (hyperthyroidism, hypothyroidism, malnutrition, dehydration) that need to be addressed.
For this reason, it’s important to always consider your personal circumstances and adopt an individual approach to treating PCOS. I highly suggest working with a professional (at least at the beginning) to fully understand your condition and find the best strategies for you.
However, most women with PCOS can successfully heal their acne by addressing and managing those three factors: insulin resistance, inflammation and chronic stress. And here’s how to do it naturally, without the use of birth control pills (or other hormonal medication).
How to treat PCOS acne naturally:
- make dietary changes
- exercise regularly
- get enough sleep
- manage stress
- eliminate environmental toxins
- quit smoking
- include dietary supplements
- use appropriate skincare
1. Diet
Your diet is perhaps the most powerful tool you can use to restore hormonal balance and get rid of acne for good. While I might be slightly biased by my nutritional background I can fully agree with the importance of diet based on my personal experience.
As I’ve already mentioned I used to suffer from severe hormonal acne for a long time, desperately trying every topical treatment I could find (I wasn’t diagnosed with PCOS at that time). However, it was only after I completely changed my diet that I started registering some major improvements in my skin.
In fact, I was so impressed by the results that I decided to study nutritional science professionally and pursue my career in this field. There really is some truth to the saying ‘you are what you eat’ since food is basically information for your body.
The role of diet
It is not surprising that different foods will act differently once they enter your body as they all consist of different chemical compounds and structures. Your food choices can, therefore, directly affect your bodily functions and overall health (including hormonal health and skin quality).
“Your food choices can directly affect your bodily functions and overall health.”
One of the main reasons why diet is such an important aspect in the management of PCOS and hormonal acne is its link to insulin resistance. That’s because insulin resistance is a condition directly affected by your blood glucose levels (too much glucose=too much insulin). And your blood glucose levels are directly affected by what you eat.
In addition, your body composition (being overweight or obese) can also affect your condition as excessive body fat (especially visceral ‘belly’ fat) contributes to insulin resistance and inflammation in the body.
Read more: ‘PCOS Belly Fat Explained & How To Reduce It’
Dietary strategies
Your diet should therefore primarily focus on blood sugar regulation and weight management if your goal is to reduce insulin resistance, androgens and PCOS acne. However, there are other nutritional strategies that can help you do that such as adopting a diet rich in anti-inflammatory, anti-oxidant and hormone-balancing foods.
Such foods can help reduce inflammation, improve insulin resistance, manage stress and balance hormones. A diet rich in certain nutrients (such as zinc, omega-3, magnesium, collagen, vitamin D) can also have a big impact on the quality of your skin and support its recovery.
On the other hand, there are some foods that may increase the risk of acne and therefore should be limited. Those foods may include dairy, gluten, alcohol, processed foods, and peanuts. According to research low GI, low-carb, dairy-free and anti-inflammatory diets appear to be best for reducing acne.
If you’d like to get more information about how to fully reverse PCOS through dietary changes, make sure to check out my detailed easy-to-follow guide here: ‘The Best PCOS Diet (Ultimate Guide)’. But here are some of the best foods you should include in your diet to heal PCOS acne.
Best foods for PCOS acne:
- Proteins (eggs, fish, meat, soy, beans, bone broth)
- Anti-inflammatory foods (whole fruits, vegetables)
- Herbs and spices (cinnamon, turmeric, spearmint, licorice)
- Healthy fats (avocado, olives, oily fish, nuts, seeds)
- Seaweed (kelp)
- Adaptogenic mushrooms (reishi, chaga)
- Natural DHT blockers (pumpkin seeds, coffee, green tea)
- Low GI foods (wholefoods, unprocessed foods)
- Herbal tea (Best Teas For PCOS)
2. Exercise
There are several different reasons why exercise is another important factor that can affect your hormonal health and skin condition. It is clear that regular exercise can help you manage weight and improve metabolism, however, it also directly impacts your body’s insulin sensitivity.
Exercise has not only an immediate effect on your insulin levels (it decreases insulin by uptaking more glucose into working muscles) but it can also significantly reduce insulin resistance over time (by making your body more sensitive to insulin).
In addition, exercise is associated with some serious benefits for mental health and stress management that can also drastically affect your hormone levels and the production of androgens.
Another great benefit of exercise for healing acne is its ability to increase blood flow to your skin cells and deliver essential nutrients. Improved blood flow to your skin also helps remove toxins, free radicals and other waste products from your cells. As a result, your skin is more likely to be well-nourished and revitalized.
Learn more about the best types of exercise for PCOS here: ‘What Is The Best Exercise For PCOS & Why?’
Does exercise help with PCOS acne?
Exercise can help reduce PCOS acne as it provides multiple benefits important for the management of this condition. It helps regulate hormones by improving insulin sensitivity, managing weight and reducing stress. Additionally, it also improves skin quality by increasing blood flow to the cells.
Best exercise for PCOS acne:
- Cardio (running, cycling, swimming, skipping, HIIT)
- Restorative exercise (yoga, pilates, walking, thai chi)
- Strength training (weightlifting, resistance bands, kettlebells)
- Sports (tennis, volleyball, hockey, soccer)
3. Sleep
If your goal is to successfully restore hormonal balance, improve skin health and reduce PCOS acne you should never underestimate the importance of sleep. That’s because sleep is involved in so many processes in your body (including regeneration, hormone regulation, detoxication, repair) that can have a huge impact on your condition.
Your sleeping habits can therefore directly affect all of the three main drivers of PCOS acne (insulin resistance, inflammation and chronic stress) as well as the quality of your skin.
Multiple studies have shown how insufficient sleep can almost immediately result in impaired metabolism and disrupted hormones (especially insulin and cortisol). Since excess insulin and cortisol levels are the main contributors to PCOS-related acne, you should always prioritize getting enough high-quality sleep.
Another thing to keep in mind is that the vast majority of your epidermis cells get repaired during sleep. It is the time when your body is able to increase blood flow to your skin, rebuild its collagen and repair any damages. In other words, you really need your beauty sleep.
4. Stress
I can confirm that keeping your stress levels in balance is one of the most difficult things to do if you suffer from PCOS and hormonal acne as it’s an extremely stressful experience. Yet, it is one of the most important factors that can drastically affect your skin health and PCOS acne.
I’ve already explained how chronic stress can increase the production of androgens in your adrenals and how increased cortisol can stimulate the oil (sebum) secretion in your skin. Since both mechanisms play a huge role in the development and progression of acne, it is essential to develop effective stress management strategies.
Unfortunately, there is no universal stress-relieving technique that would work for everyone as we all experience different triggers and respond to different strategies. For this reason, it’s important you try different methods and find the ones that work for you.
Meditation, breathing exercises, yoga and spending time in nature appear to be some of the most effective methods for lowering cortisol levels, according to research. So you may want to start there.
5. Environmental toxins
Increased exposure to environmental toxins has been identified as a major risk factor for developing PCOS. This is particularly true for a group of toxins called EDCs (endocrine-disrupting chemicals).
Such chemicals can mimic, block and interfere with your hormones once they enter your body which can lead to hormone imbalances and endocrine disorders (such as PCOS). EDCs have been also shown to affect fertility, insulin resistance and hyperandrogenism in women with PCOS.
While it is almost impossible to completely eliminate your exposure to EDCs in today’s environment, you should aim to minimize your contact with those toxins as much as possible. EDCs can be found everywhere from the food we eat and water we drink to the air we breathe and products we use (packaging, plastics, cosmetics, toys).
If your goal is to heal PCOS acne and restore hormonal balance I highly suggest going through your everyday-use items and finding better alternatives. In terms of your diet, you can minimize your exposure to EDCs by:
- buying organic foods
- choosing EDCs-free packaging
- filtering your water
- storing food in EDCs-free containers
However, you should pay especially close attention to your skincare and haircare products, perfumes and make-up as they’re usually filled with EDCs that you put in direct contact with your skin (some of my favorite EDCs-free skincare products are listed later in this post).
6. Smoking
While smoking is generally not considered healthy for anyone, women with PCOS may suffer even greater consequences from this habit. That’s because there’s a close link between smoking, PCOS and acne.
According to studies, smoking cigarettes increases the risk of insulin resistance, inflammation and metabolic syndrome. Increased androgens levels in women have also been associated with smoking cigarettes and nicotine. For this reason, smoking is considered a major risk factor for hyperandrogenism and PCOS.
Read more: ‘Does Smoking Affect PCOS & How? All You Need To Know‘
Additionally, there is also evidence that smoking may contribute to post-adolescence acne and inflammatory skin diseases. Smoking can also seriously impact the quality of your skin as it reduces blood flow, speeds up aging and slows down the healing process.
For this reason, it is best to avoid smoking completely if you suffer from PCOS as you’re more likely to restore your hormonal balance, reduce acne and improve your skin condition.
7. Supplements
Dietary supplements are another effective tool that can help you successfully balance hormones, reduce acne and improve your skin quality. However, there are a few important things to consider when it comes to supplements.
First of all, keep in mind that supplements are not a cure that would work miracles on their own. While they can be extremely helpful in the management of PCOS and hormonal acne they should be used only as additional support to your diet and not as your primary treatment strategy. Dietary and lifestyle habits should always remain your priority.
Secondly, you want to be extra selective with your supplements as they’re not strictly regulated by governmental bodies (such as FDA) and their content is not always guaranteed. As a result. it can become really difficult to find dietary supplements that are actually effective.
“Supplements are not strictly regulated by governmental bodies and their content is not always guaranteed.”
Another thing to be aware of is that PCOS is a very complex condition that we all experience differently. This means that the effects of different supplements may vary between individuals based on their unique conditions and causes of PCOS acne.
For this reason, I highly suggest obtaining as much data about your condition as possible (such as bloodwork, tests, health assessments) or working with a professional. Once you fully understand your condition it is much easier to develop relevant strategies and supplement plans specifically tailored to your needs.
While a personalized approach in the treatment of PCOS is extremely important (in my opinion) I understand that it may not be accessible to all. Therefore, I’ve created a list of the most effective supplements and herbal remedies for PCOS acne based on the current evidence as well as my personal experience.
Best supplements for PCOS acne:
- Inositol
- Omega-3
- Zinc
- Vitamin D
- Magnesium
- Probiotics
- Collagen
- Berberine
- Saw palmetto
- Vitex
- Primrose evening oil
- Green tea
- Spearmint
a) Hormone-regulators
Since hormone imbalance, hyperandrogenism and insulin resistance are the main drivers of acne in most women with PCOS it is clear that some of the most effective supplements for acne will target those causes.
• Insulin resistance
Berberine and inositol supplements have been shown to be particularly effective in improving insulin resistance in women with PCOS. Their effects were comparable to metformin (a blood sugar-lowering drug) and several studies even registered improvements in acne at the end of the trials.
• DHT blockers
Other powerful supplements for acne are those that are able to lower androgens in the blood, specifically DHT. There are a few supplements and herbs that have been shown to block the production of DHT by inhibiting the enzyme 5-AR (5-alpha reductase) which is responsible for converting testosterone to DHT.
Some of the most powerful natural DHT blockers include green tea extract, saw palmetto, spearmint, stinging nettle and pumpkin seed oil. Those compounds are also commonly combined into one product to create more effective DHT-blocking formulas.
• Progesterone regulation
Vitex (Chasteberry) has also been shown to improve acne in multiple studies which is believed to be due to its hormone-balancing effects. Vitex appears to naturally increase the levels of progesterone that is involved in skin health. Another supplement that is associated with similar beneficial effects on progesterone and female hormones is evening primrose oil.
Here are some of my favorite brands:
- Berberine by Thorne Research (available on Amazon)
- Inositol Powder by Theralogix (available on Amazon)
- Natural DHT Blocker by Herbtonics (available on Amazon)
- Spearmint Tea by FGO (available on Amazon)
- Saw Palmetto by Havasu Nutrition (available on Amazon)
- Vitex by Nature’s Way (available on Amazon)
- Evening Primrose Oil by Sports Research (available on Amazon)
b) Nutrients
Another important thing to consider is consuming sufficient amounts of nutrients essential for skin health and recovery through your diet and/or through supplementation.
• Essential nutrients
There are many essential nutrients involved in skin health and skin quality. According to research, some of the most vital ones include zinc, vitamin D, magnesium and omega-3. Deficiencies in those nutrients have been associated with an increased risk of acne in multiple studies.
You can easily obtain most of those nutrients from a healthy balanced diet (and sun exposure), however, additional supplementation can still be extremely valuable (and sometimes necessary) for a lot of women with PCOS acne.
• Probiotics & collagen
Supplementing with probiotics and collagen may also help reduce acne and improve skin health as it’s been demonstrated in several studies. Just remember the ‘food first’ approach, get your blood levels tested and always look for high-quality supplements from reliable sources with a third-party certification.
Here are some of my favorite brands:
- Vitamin D3 by Naturewise (available on Amazon)
- Zinc by Solgar (available on Amazon)
- Omega-3 by Nordic Naturals (available on Amazon)
- Magnesium by Doctor’s Best (available on Amazon)
- Probiotics by Garden of Life (available on Amazon)
- Collagen Powder by Ancient Nutrition (available on Amazon)
For more tips on how to best choose and use protein powders for PCOS, make sure to check out my previous article ‘What Protein Powder Is Best For PCOS? (The Ultimate Guide)‘.
8. Skincare
Even though the root cause of PCOS acne is hormone-related and should be primarily treated from the inside out, your skincare is still extremely important. How you care for your skin and what topical products you use can also make a huge difference.
While most topical treatments are not able to fully heal hormonal acne, they can help reduce bacteria, lower inflammation, increase hydration and speed up the recovery process. On the other hand, inappropriate skincare may be irritating to your skin that can lead to even worse acne and decreased skin quality.
Just keep in mind that your skincare is only a part of the equation and that there is no magical topical treatment that makes hormonal acne go away. Practicing appropriate skincare is very important but balancing your hormones through dietary and lifestyle changes (discussed above) is the real key.
Best skincare products for PCOS acne:
- Oil-free Moisturizer
- Sulfur Soap
- Zinc Diaper Cream
- Bentonite Clay Mask
- Activated Charcoal
- Tee-tree Oil
- Aloe Vera Gel
- Hyaluronic Acid
- Nizoral
- Benzoyl Peroxide
- Witch Hazel
- LED Light Therapy Mask
- Facial Cleansing Brush
You can find a detailed list of all of my favorite skincare products here: ‘The Best Skincare Products For PCOS & Hormonal Acne‘ but here’s a summary of some of the most important ones.
a) Skincare cosmetics
While I believe that finding the right skincare products is extremely individual (as we all have very unique skin), there are a few things you should consider if you suffer from PCOS acne.
• Endocrine disruptors
The first thing to keep in mind when it comes to choosing the right skincare for PCOS acne is to avoid any products that may contain endocrine-disrupting chemicals (EDCs). Most commercial products are filled with artificial chemicals, perfumes, parabens and silicons that can easily enter your bloodstream through skin pores and cause hormone imbalances.
Therefore, it is better to opt for organic products with natural ingredients since you’ll be using them on a daily basis. You may also want to choose products (especially moisturizers) that are oil-free to prevent the growth of bacteria in your skin and clogged pores.
• Sensitivity
Because our skin is usually sensitive to different ingredients, finding the right products is a very personal task. Therefore, it’s important to understand how you react to different substances (you can keep a skin diary) and then choose your products accordingly (use online ingredient checkers).
I personally have very sensitive skin and it’s always difficult for me to find products that wouldn’t make my skin irritated, dry and red. That’s why I keep my skincare extremely simple and use only a few products that I can tolerate.
• Bacteria overgrowth
I highly recommend looking for products that are specifically developed for ‘seborrheic dermatitis’ as they really help prevent the acne from spreading. You can also look for products that contain sulfur or ichthammol (I like soaps) as those ingredients are very effective in reducing the growth of bacteria and oil production on your skin.
• Scars
In terms of reducing redness and healing acne scarring, I had the best result with using products containing zinc (such as diaper creams), hyaluronic acid and kojic acid. Keeping your skin hydrated and moisturized is also really important as it speeds up the healing process.
Here are some of my favorite brands:
- Oil-free Moisturizer by Honest Beauty (available on Amazon)
- Sulfur Soap by Joesoef Skincare (available on Amazon)
- Zinc Diaper Cream by Carell (available on Amazon)
- Hyaluronic Acid by Cosmedica Skincare (available on Amazon)
- Brightening Mask by Lather (available on Amazon)
b) Topical treatments
There are a few products that work really well for reducing severe and very inflamed acne, however, those products can be very aggressive to your skin and should be used with extra caution. I don’t recommend using those products on a regular basis but rather only in case of emergencies.
• Nizoral
Nizoral (an anti-dandruff shampoo) is very effective in reducing inflammation and bacteria in your skin. However, you should only leave it on for a short period of time as it could seriously damage your skin (especially on your face). You can use it as a ‘face wash’ a couple of times a week or as a ’face mask’ for no longer than 5-10 minutes. Just don’t overuse it!
• Benzoyl peroxide
Benzoyl peroxide is another powerful antiseptic ingredient that helps inhibits the growth of bacteria and stop acne from spreading. However, it too can be very drying and irritating to your skin when used in excessive amounts or too frequently. Opt for the lower-concentrated gels and use it only on the affected area rather than your full face.
• Salicylic acid
Another powerful anti-inflammatory ingredient often added to topical acne treatments is salicylic acid. Salicylic acid helps exfoliate the skin by breaking down dead skin cells and sebum oils. However, this ingredient is poorly tolerated by many individuals and can lead to skin irritations when used too frequently.
Here are some of my favorite brands:
- Anti-dandruff Shampoo by Nizoral (available on Amazon)
- Benzoyl Peroxide Gel by Proactive (available on Amazon)
- Salicylic Acid Exfoliant by Paula’s Choice (available on Amazon)
c) Natural remedies
As I’ve already mentioned I like to keep my skincare very simple and stick to natural ingredients most of the time. Some of my favorite skincare products are actually a single ingredient.
• Make-up remover
For example, I use pure coconut oil as a make-up remover as it doesn’t irritate my eyes and it removes make-up really well. You can also use other natural oils to remove make-up (such as hemp, argan, olive) however I don’t find them as practical as coconut oil. Just make sure you double cleanse your face afterward to prevent any oil build-up.
• Toner
Witch hazel is my go-to natural toner as it’s not drying and it doesn’t make my skin go red. Apple cider vinegar also works as a natural toner good for reducing acne, however, you should always dissolve it in water as it can be too aggressive to your skin (it’s an acid after all). It also doesn’t smell particularly nice so I don’t recommend using it on a daily basis.
• Face mask
Some of my favorite ingredients for making homemade face masks are bentonite clay and activated charcoal. You can buy those in powdered forms and just mix them with water or some other additional ingredients.
They really clean your pores in depth and remove excess oils, however, they can be very drying (make sure you moisturize afterward). You can also use pure aloe vera gel as a face mask to boost hydration and reduce blemishes.
• Essential oils
I also like using essential oils in my skincare as some of them are particularly beneficial for treating acne. Tea tree oil is perhaps the most popular one as it has strong anti-inflammatory and anti-bacterial properties. It is backed by research and it really works wonders when applied directly on spots.
However, using 100% tea tree oil may cause redness and irritations in over-sensitive skin which is why you may need to dissolve it in water first. I recommend using cotton swabs for easier application (dip it in water first and then add a few drops of tea tree oil).
Some of my other favorite essential oils for skincare include lavender and frankincense. Those are not as effective as a direct spot treatment but they work well for reducing blemishes, improving skin texture and fading acne scars. Try mixing a few drops into your daily moisturizer or add them to your homemade face masks.
Here are some of my favorite brands:
- Bentonite Clay Mask by Aztec Secret (available on Amazon)
- Activated Charcoal by Viva Doria (available on Amazon)
- Organic Tea Tree Oil by Cliganic (available on Amazon)
- Witch Hazel Toner by Thayers (available on Amazon)
- Organic Aloe Vera Gel by Seven Minerals (available on Amazon)
d) Skincare tools
In addition to topical products, there are other ways in which you can improve the quality of your skin and reduce acne. Some of the most effective ones include massage, light therapy and microneedeling.
• Massage
Massaging your skin can be extremely beneficial as it increases blood flow, improves elasticity and stimulates the production of collagen. You can easily do this with your hands and fingers but there are also some practical tools that make this process much easier such as gua sha or jade roller (my favorites).
I also highly recommend getting your hands on one of the electric facial cleansing brushes. They really do cleanse your skin in more depth (especially great if you wear make-up on a daily basis) but they also work well as a face massager.
• Light therapy
Light therapy (especially red and blue) is also now increasing in popularity as it’s becoming more researched and accessible for regular use. Red light appears to have anti-inflammatory and tissue-repairing effects as it’s able to go deep below your skin surface. It is primarily used to promote healing and reduce acne scarring.
Blue light is mostly associated with strong anti-bacterial properties that help prevent acne from spreading. It also appears to reduce the production of sebum which is responsible for clogged pores and acne development. According to studies, a combination of red and blue light provides the most benefits for individuals suffering from acne.
Fortunately, there are now many home devices that offer a combination of red and blue light such as light therapy masks, wands or panels. I personally use my light therapy mask on a regular basis as I find that it helps even out my skin tone and fade acne scars. I also find it very relaxing.
• Microneedling
Another great technique that helps fade acne scars and stimulate collagen production is microneedling which is now also widely available for home use. However, I don’t recommend using this method if you still suffer from active and inflamed acne as it may increase the risk of infection.
Here are some of my favorite brands:
- LED Light Therapy Mask by Aphrona (available on Amazon)
- Guasha & Jade Roller Set by BAIMEI (available on Amazon)
- Facial Cleansing Brush by Vanity Planet (available on Amazon)
- Foreo Luna 3 by Foreo (available on Amazon)
- Microneedling Derma Roller by Sdara (available on Amazon)
Practical tips
- Go to saunas – heat exposure is associated with numerous health benefits and it’s particularly beneficial for your skin, it helps boost blood flow, remove toxins and make your skin ‘glow’ + infrared saunas have additional light therapy benefits
- Do handstands – handstands and inversions are another great way to increase blood flow to your skin cells, deliver more nutrients and speed up the healing process
- Use ingredient checkers – you can check the content of almost any product online to find any potential endocrine disruptors, allergens or other irritating ingredients, I like using INCIDecoder and Sezia for skincare
- Change pillowcases – make sure you change your pillowcases frequently to prevent spreading bacteria on your skin, your pillow is one of the most bacteria-friendly places as it’s usually covered in sweat, oils, dirt and dead skin
- Don’t touch your face – perhaps the most difficult but the most important thing is not touching and picking your face, but it really stops bacteria from spreading and helps prevent infection and scarring
- Clean your phone – your phone is another common home for various bacteria that can easily spread onto your skin, make sure you clean it frequently and try not to hold it close to your face when on the phone
- Use clean face towels – use separate towels for your face and change them frequently, you can get 7 mini towels (1 for each day) for your face and wash them all once a week
- Clean your make-up brushes – keep your make-up brushes clean and make sure you wash them frequently since it’s something you put directly on your face every day
- Have makeup-free days – even though it’s hard to stay away from any coverage if you suffer from problematic skin (trust me I know), it is important to allow your skin to fully breathe and recover, try having at least a few makeup-free days a week and opt for non-toxic makeup products, you can find my favorite ones here: ‘The Best Makeup Products For PCOS & Hormonal Acne‘.
- Exfoliate gently – exfoliating is important for removing dead skin cells and cleaning your pores but you shouldn’t overdo it or be too aggressive as it can irritate your skin and lead to even worse acne (exfoliate 1-2x per week very gently)
- Get tested – get your hormones and other important health metrics tested regularly so you can better understand your condition, find appropriate treatment strategies and track your progress
- Be patient – keep in mind that our endocrine system is very complex and once you introduce new treatment strategies, it usually takes a minimum of 3-6 months before you start seeing some results (especially when healing your skin)
Resources:
- Andreasen, A. S., Larsen, N., Pedersen-Skovsgaard, T., Berg, R. M., Møller, K., Svendsen, K. D., Jakobsen, M., & Pedersen, B. K. (2010). Effects of Lactobacillus acidophilus NCFM on insulin sensitivity and the systemic inflammatory response in human subjects. The British journal of nutrition, 104(12), 1831–1838. https://doi.org/10.1017/S0007114510002874
- Archer, J. S., & Chang, R. J. (2004). Hirsutism and acne in polycystic ovary syndrome. Best practice & research. Clinical obstetrics & gynaecology, 18(5), 737–754. https://doi.org/10.1016/j.bpobgyn.2004.05.007
- Bae, Y. S., Hill, N. D., Bibi, Y., Dreiher, J., & Cohen, A. D. (2010). Innovative uses for zinc in dermatology. Dermatologic clinics, 28(3), 587–597. https://doi.org/10.1016/j.det.2010.03.006
- Capitanio, B., Sinagra, J. L., Ottaviani, M., Bordignon, V., Amantea, A., & Picardo, M. (2009). Acne and smoking. Dermato-endocrinology, 1(3), 129–135. https://doi.org/10.4161/derm.1.3.9638
- Clark, A. K., Haas, K. N., & Sivamani, R. K. (2017). Edible Plants and Their Influence on the Gut Microbiome and Acne. International journal of molecular sciences, 18(5), 1070. https://doi.org/10.3390/ijms18051070
- Fabbrocini, G., Bertona, M., Picazo, Ó., Pareja-Galeano, H., Monfrecola, G., & Emanuele, E. (2016). Supplementation with Lactobacillus rhamnosus SP1 normalises skin expression of genes implicated in insulin signalling and improves adult acne. Beneficial microbes, 7(5), 625–630. https://doi.org/10.3920/BM2016.0089
- Faghfoori, Z., Fazelian, S., Shadnoush, M., & Goodarzi, R. (2017). Nutritional management in women with polycystic ovary syndrome: A review study. Diabetes & metabolic syndrome, 11 Suppl 1, S429–S432. https://doi.org/10.1016/j.dsx.2017.03.030
- Fouladi R. F. (2012). Aqueous extract of dried fruit of Berberis vulgaris L. in acne vulgaris, a clinical trial. Journal of dietary supplements, 9(4), 253–261. https://doi.org/10.3109/19390211.2012.726702
- Gao, H., Geng, T., Huang, T., & Zhao, Q. (2017). Fish oil supplementation and insulin sensitivity: a systematic review and meta-analysis. Lipids in health and disease, 16(1), 131. https://doi.org/10.1186/s12944-017-0528-0
- González-Saldivar, G., Rodríguez-Gutiérrez, R., Ocampo-Candiani, J., González-González, J. G., & Gómez-Flores, M. (2017). Skin Manifestations of Insulin Resistance: From a Biochemical Stance to a Clinical Diagnosis and Management. Dermatology and therapy, 7(1), 37–51. https://doi.org/10.1007/s13555-016-0160-3
- Grant, P., & Ramasamy, S. (2012). An update on plant derived anti-androgens. International journal of endocrinology and metabolism, 10(2), 497–502. https://doi.org/10.5812/ijem.3644
- Housman, E., & Reynolds, R. V. (2014). Polycystic ovary syndrome: a review for dermatologists: Part I. Diagnosis and manifestations. Journal of the American Academy of Dermatology, 71(5), 847.e1–858. https://doi.org/10.1016/j.jaad.2014.05.007
- Ju, Q., Tao, T., Hu, T., Karadağ, A. S., Al-Khuzaei, S., & Chen, W. (2017). Sex hormones and acne. Clinics in dermatology, 35(2), 130–137. https://doi.org/10.1016/j.clindermatol.2016.10.004
- Juhl, C. R., Bergholdt, H., Miller, I. M., Jemec, G., Kanters, J. K., & Ellervik, C. (2018). Dairy Intake and Acne Vulgaris: A Systematic Review and Meta-Analysis of 78,529 Children, Adolescents, and Young Adults. Nutrients, 10(8), 1049. https://doi.org/10.3390/nu10081049
- Kandaraki, E., Chatzigeorgiou, A., Livadas, S., Palioura, E., Economou, F., Koutsilieris, M., Palimeri, S., Panidis, D., & Diamanti-Kandarakis, E. (2011). Endocrine disruptors and polycystic ovary syndrome (PCOS): elevated serum levels of bisphenol A in women with PCOS. The Journal of clinical endocrinology and metabolism, 96(3), E480–E484. https://doi.org/10.1210/jc.2010-1658
- Kucharska, A., Szmurło, A., & Sińska, B. (2016). Significance of diet in treated and untreated acne vulgaris. Postepy dermatologii i alergologii, 33(2), 81–86. https://doi.org/10.5114/ada.2016.59146
- Lee, Y. B., Byun, E. J., & Kim, H. S. (2019). Potential Role of the Microbiome in Acne: A Comprehensive Review. Journal of clinical medicine, 8(7), 987. https://doi.org/10.3390/jcm8070987
- Leproult, R., & Van Cauter, E. (2010). Role of sleep and sleep loss in hormonal release and metabolism. Endocrine development, 17, 11–21. https://doi.org/10.1159/000262524
- Lim, S. K., Ha, J. M., Lee, Y. H., Lee, Y., Seo, Y. J., Kim, C. D., Lee, J. H., & Im, M. (2016). Comparison of Vitamin D Levels in Patients with and without Acne: A Case-Control Study Combined with a Randomized Controlled Trial. PloS one, 11(8), e0161162. https://doi.org/10.1371/journal.pone.0161162
- Lu, P. H., & Hsu, C. H. (2016). Does supplementation with green tea extract improve acne in post-adolescent women? A randomized, double-blind, and placebo-controlled clinical trial. Complementary therapies in medicine, 25, 159–163. https://doi.org/10.1016/j.ctim.2016.03.004
- Marx, T. L., & Mehta, A. E. (2003). Polycystic ovary syndrome: pathogenesis and treatment over the short and long term. Cleveland Clinic journal of medicine, 70(1), 31–45. https://doi.org/10.3949/ccjm.70.1.31
- Moran, L. J., Hutchison, S. K., Norman, R. J., & Teede, H. J. (2011). Lifestyle changes in women with polycystic ovary syndrome. The Cochrane database of systematic reviews, (2), CD007506. https://doi.org/10.1002/14651858.CD007506.pub2
- Nadjarzadeh, A., Dehghani Firouzabadi, R., Vaziri, N., Daneshbodi, H., Lotfi, M. H., & Mozaffari-Khosravi, H. (2013). The effect of omega-3 supplementation on androgen profile and menstrual status in women with polycystic ovary syndrome: A randomized clinical trial. Iranian journal of reproductive medicine, 11(8), 665–672. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3941370/
- Nasri, K., Akrami, S., Rahimi, M., Taghizadeh, M., Behfar, M., Mazandaranian, M. R., Kheiry, A., Memarzadeh, M. R., & Asemi, Z. (2018). The effects of vitamin D and evening primrose oil co-supplementation on lipid profiles and biomarkers of oxidative stress in vitamin D-deficient women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Endocrine research, 43(1), 1–10. https://doi.org/10.1080/07435800.2017.1346661
- Papalou, O., & Diamanti-Kandarakis, E. (2017). The role of stress in PCOS. Expert review of endocrinology & metabolism, 12(1), 87–95. https://doi.org/10.1080/17446651.2017.1266250
- Pappas A. (2009). The relationship of diet and acne: A review. Dermato-endocrinology, 1(5), 262–267. https://doi.org/10.4161/derm.1.5.10192
- Pau, C. T., Keefe, C. C., & Welt, C. K. (2013). Cigarette smoking, nicotine levels and increased risk for metabolic syndrome in women with polycystic ovary syndrome. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 29(6), 551–555. https://doi.org/10.3109/09513590.2013.788634
- Pei, S., Inamadar, A. C., Adya, K. A., & Tsoukas, M. M. (2015). Light-based therapies in acne treatment. Indian dermatology online journal, 6(3), 145–157. https://doi.org/10.4103/2229-5178.156379
- Ramezani Tehrani, F., Behboudi-Gandevani, S., Bidhendi Yarandi, R., Saei Ghare Naz, M., & Carmina, E. (2021). Prevalence of acne vulgaris among women with polycystic ovary syndrome: a systemic review and meta-analysis. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 37(5), 392–405. https://doi.org/10.1080/09513590.2020.1859474
- Roudsari, M. R., Karimi, R., Sohrabvandi, S., & Mortazavian, A. M. (2015). Health effects of probiotics on the skin. Critical reviews in food science and nutrition, 55(9), 1219–1240. https://doi.org/10.1080/10408398.2012.680078
- Saric, S., Notay, M., & Sivamani, R. K. (2016). Green Tea and Other Tea Polyphenols: Effects on Sebum Production and Acne Vulgaris. Antioxidants (Basel, Switzerland), 6(1), 2. https://doi.org/10.3390/antiox6010002
- Schrom, K. P., Ahsanuddin, S., Baechtold, M., Tripathi, R., Ramser, A., & Baron, E. (2019). Acne Severity and Sleep Quality in Adults. Clocks & sleep, 1(4), 510–516. https://doi.org/10.3390/clockssleep1040039
- Shele, G., Genkil, J., & Speelman, D. (2020). A Systematic Review of the Effects of Exercise on Hormones in Women with Polycystic Ovary Syndrome. Journal of functional morphology and kinesiology, 5(2), 35. https://doi.org/10.3390/jfmk5020035
- Smith, R. N., Mann, N. J., Braue, A., Mäkeläinen, H., & Varigos, G. A. (2007). A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. The American journal of clinical nutrition, 86(1), 107–115. https://doi.org/10.1093/ajcn/86.1.107
- Stewart, T. J., & Bazergy, C. (2018). Hormonal and dietary factors in acne vulgaris versus controls. Dermato-endocrinology, 10(1), e1442160. https://doi.org/10.1080/19381980.2018.1442160
- Thiboutot, D., Harris, G., Iles, V., Cimis, G., Gilliland, K., & Hagari, S. (1995). Activity of the type 1 5 alpha-reductase exhibits regional differences in isolated sebaceous glands and whole skin. The Journal of investigative dermatology, 105(2), 209–214. https://doi.org/10.1111/1523-1747.ep12317162
- Unfer, V., Facchinetti, F., Orrù, B., Giordani, B., & Nestler, J. (2017). Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine connections, 6(8), 647–658. https://doi.org/10.1530/EC-17-0243
- Zacchè, M. M., Caputo, L., Filippis, S., Zacchè, G., Dindelli, M., & Ferrari, A. (2009). Efficacy of myo-inositol in the treatment of cutaneous disorders in young women with polycystic ovary syndrome. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 25(8), 508–513. https://doi.org/10.1080/09513590903015544
- Zaenglein, A. L., Pathy, A. L., Schlosser, B. J., Alikhan, A., Baldwin, H. E., Berson, D. S., Bowe, W. P., Graber, E. M., Harper, J. C., Kang, S., Keri, J. E., Leyden, J. J., Reynolds, R. V., Silverberg, N. B., Stein Gold, L. F., Tollefson, M. M., Weiss, J. S., Dolan, N. C., Sagan, A. A., Stern, M., … Bhushan, R. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology, 74(5), 945–73.e33. https://doi.org/10.1016/j.jaad.2015.12.037
- Zari, S., & Alrahmani, D. (2017). The association between stress and acne among female medical students in Jeddah, Saudi Arabia. Clinical, cosmetic and investigational dermatology, 10, 503–506. https://doi.org/10.2147/CCID.S148499
