If you have PCOS (Polycystic Ovary Syndrome) you may as well be insulin resistant. But what exactly is insulin resistance and how is it linked to the syndrome?
PCOS is a complex endocrine disorder and despite the growing number of studies researching this condition, the origin of PCOS remains unclear without one single cause identified. In fact, it is suggested that PCOS results from the interaction of multiple different factors including genes, environment, and lifestyle.
While there are different explanations and theories for the condition development, there is one aspect that seems to play a key role in PCOS and it is insulin.
What is insulin?
Insulin is a hormone produced by your pancreas and its main role is to regulate your blood sugar (glucose) levels. The way it works is that insulin (acting as a key) lets glucose from your bloodstream into your cells so it can be used for energy.
The aim of your body is to always keep your blood glucose levels in a steady state (approx. 4g of glucose in your blood) and by using different mechanisms and hormones (including insulin), it’s constantly working to maintain this balance.
Your body releases insulin in response to increased levels of glucose in your blood which happens after you eat any food containing carbohydrates. In normal circumstances, your body is highly efficient in this process which keeps your glucose levels regulated and everything functioning properly.
However, there are cases in which this process doesn’t function properly causing a series of other issues and disruptions in your metabolism. One of those metabolic dysfunctions is called ‘Insulin Resistance’ and more and more studies now recognize it to be closely linked to PCOS.
What is insulin resistance?
Insulin resistance is a condition when your cells stop responding to insulin effectively and your body is unable to decrease your blood sugar levels (by letting glucose into your cells).
But high blood glucose levels signal to your pancreas to release even more insulin so you can easily end up with hyperinsulinemia (high insulin levels in your blood).
As you can imagine, having high levels of insulin in your blood is not ideal and if unregulated, it can have some tremendous health consequences. But how exactly is it linked to PCOS?
The link between PCOS and insulin resistance
One of the impacts of high levels of insulin (hyperinsulinemia) in your blood is that it can make your ovaries (which have insulin receptors) increase the production of androgens (male hormones). High levels of androgens cause many of the common PCOS symptoms such as acne, oily skin, hair loss, hirsutism, and missing periods.
But high levels of insulin also prevent your body from breaking down fat and using it for energy, which is why it’s so difficult to lose weight if you have PCOS.
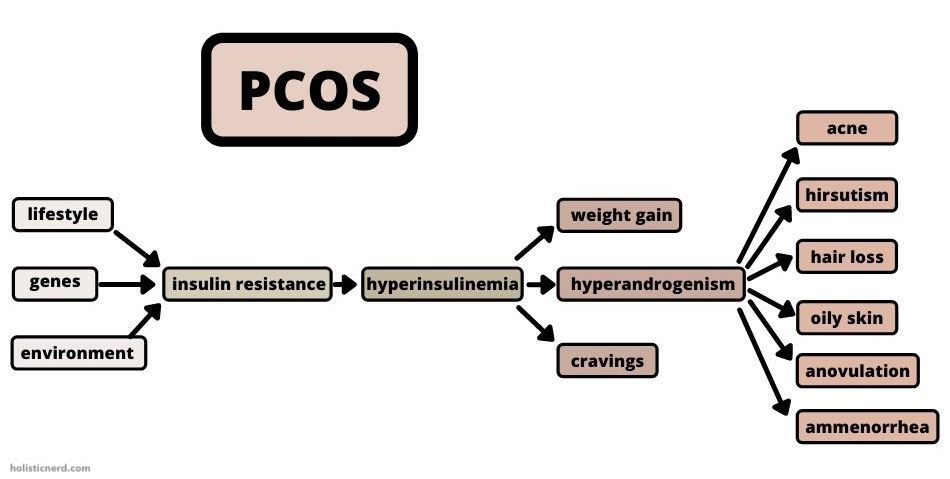
Insulin is also an appetite stimulant that may lead to weight gain and excessive fat. Unfortunately, excessive fat is also one of the contributors to increased insulin production and insulin resistance development so the process goes around in a circle.
While high levels of insulin are oftentimes recognized as one of the symptoms of PCOS (up to 75-95% of women with PCOS are insulin resistant), it’s becoming more clear that it actually may be one of the root causes of the condition driving all of the other symptoms.
Risks of insulin resistance
If you are insulin resistant it basically means that you are pre-diabetic (your blood sugar levels are higher than normal). This puts you at a higher risk of developing type 2 diabetes in which case your body becomes even less efficient in regulating insulin.
Type 2 diabetes is a serious chronic condition leading to some serious long-term consequences (cardiovascular disease, kidney damage, vision problems, nerve damage).
Unfortunately, up to 50% of women with PCOS actually develop type 2 diabetes before turning 40. That’s why you should pay close attention to insulin resistance and its proper management if you suffer from PCOS.
How do I know if I’m insulin resistant?
The best way to check whether you’re insulin resistant is to get a blood test assessing your body’s ability to process sugars via fasting glucose plasma test (FGP) or oral glucose tolerance test (OGTT).
- The FGP test will only measure your glucose levels in a fasted state and based on the results will consider your levels normal (<100mg/dL), pre-diabetic (100-125mg/dL), or diabetic (>125mg/dL).
- The OGTT test will also measure your glucose levels in a fasted state but after 2 hours and eating 75 grams of sugar, another blood sample will be taken to measure your glucose levels again determining whether it’s normal (<140mg/dL), pre-diabetic (140-199mg/dL), or diabetic (<200mg/dL).
The OGTT method is considered more accurate because it measures your body’s reaction to sugar after a meal but on the other hand, it’s also more expensive, time-consuming, and in most cases less accessible.
Both tests are able to diagnose insulin resistance and you can arrange them with your doctor or another medical professional.
Screening for insulin resistance
You can also look for some signs indicating insulin resistance such as low energy, constant cravings, belly fat, skin tags, high blood pressure. However, blood tests are the most reliable method to confirm this condition and if you have PCOS I highly suggest you get screened for insulin resistance regularly.
Be aware that screening for insulin resistance in PCOS women isn’t common practice in all places (even though it’s suggested by many studies). You may need to ask for such tests yourself (as I did) or find different resources.
Don’t be afraid to reach for help from multiple professionals and get opinions from people with different backgrounds including medical doctors, naturopaths, or nutritionists.
How can I reverse insulin resistance with PCOS?
If you have PCOS and you have been diagnosed with insulin resistance, there’s actually a lot of things you can do to reverse this condition and improve your health.
Insulin resistance in women with PCOS can be effectively managed and reversed by various lifestyle modifications including weight loss, diet, exercise, sleep, and stress management.
There is a lot of scientific evidence supporting the beneficial effects of lifestyle changes on insulin resistance and PCOS symptoms, however, it’s important to always consult the options with your doctor as in some severe cases medication might be needed.
Factors affecting insulin resistance:
- Weight loss
- Diet
- Intermittent Fasting
- Exercise
- Sleep
- Stress management
1. Weight Loss
How does body fat affect insulin resistance?
If you are overweight or obese, weight loss is usually recommended to decrease insulin resistance because excessive body fat plays a major role in the condition’s development.
Adipose fat tissues don’t only release more insulin into your blood, but they also release multiple other chemical compounds (hormones, glycerols, pro-inflammatory cytokines, non-esterified fatty acids) which have been found to be contributing to insulin resistance development.
Many studies have found that even small weight loss (5-7%) can significantly reduce the risks of developing type 2 diabetes (by 58%) and improve insulin sensitivity. Studies in overweight women with PCOS have also found weight loss to be a highly effective strategy for improving their symptoms.
Choosing the right weight loss method
When it comes to weight loss, there are so many different techniques you can use to get to your ideal body composition. BUT! It is important to choose the right method which won’t actually end up with the reverse effects and repeated weight gain.
For this reason, losing weight shouldn’t be your ultimate goal but you should rather focus on maintaining a healthy weight long-term. This means that any highly restricted diets or other extreme weight loss methods (usually promising quick effects) won’t have the same results as lifestyle changes that you’ll be able to stick to for good.
Can I be insulin resistant with normal weight?
If you have PCOS and you’re not overweight or obese, you can still suffer from insulin resistance. So it’s important you get your blood sugar levels checked anyway because not many physicians will actually suggest it if your BMI (Body Mass Index) is considered normal.
If you have a healthy weight, there is still a chance that you have increased visceral fat in your body. Visceral fat (also known as belly fat) can be really dangerous to your health as it sits around your organs and can release the same chemical compounds to your blood contributing to insulin resistance.
One of the signs of increased visceral fat is having a relatively slim body with a bigger belly (body type known as skinny fat). In this situation, your goal may not be general weight loss but you want to focus on changing your body composition (losing fat, gaining muscle) to improve your health and reduce insulin resistance.
Read more: ‘PCOS Belly Fat Explained & How To Reduce It‘
2. Diet
How does diet affect insulin resistance?
Changing your diet is probably the most effective strategy to combat insulin resistance for a number of reasons. Firstly, with an appropriate diet, you’ll be able to lose weight and change your body composition which is (as you now know) super important for insulin resistance management.
But it’s not all about calories in and calories out and the type of food you eat actually matters. All food you eat consists of different macronutrients (carbohydrates, protein, fat), and each of those macronutrients will all act differently once in the body.
“The type of food you eat actually matters.”
The role of carbohydrates
Dietary protein (made of amino acids) and dietary fat (made of fatty acids) won’t naturally spike your blood sugar levels but when you consume carbohydrates (made from sugar molecules), your glucose levels will go up and your body will release insulin to bring them back down.
So when it comes to insulin resistance and an effective diet, you really want to put your focus on your carbohydrate intake.
Low-carb and keto diets are very popular and also very effective in reversing insulin resistance but they may not be sustainable for everyone. Fortunately, you don’t have to go to extremes and cut out all the carbs completely from your diet. That’s because not all carbs are created equal.
Different types of carbohydrates
Different types of carbohydrates will have different effects on your glucose levels. By recognizing those types and choosing the more “blood sugar levels friendly“, you’ll be still able to include them in your diet (and you should as most fruit and vegetables consist of carbs).
‘Carbohydrate’ is actually a very wide term including multiple different compounds all having different chemical structure, characteristics and acting differently in your body. That’s why there are so many different names and classifications for carbohydrates, which can make appropriate dietary choices a bit overwhelming.
However, if you are insulin resistant and you want to include carbohydrates in your diet, you want to look at carbs in terms of their effects on your blood sugar levels. This means how much and how quickly they spike your blood sugar levels after you eat them. If you look at carbohydrates this way you can classify them as simple carbs (sugars), complex carbs (starch), and fiber.

• Simple carbohydrates
As you can imagine, simple carbs (made out of simple sugar molecules) are very easily absorbed into your bloodstream causing your glucose levels to go immediately up. However, these rapid spikes can put a lot of stress on your pancreas making them overproduce insulin (to keep up with the sugar) or shut down completely over time (developing diabetes).
It also makes your cells less sensitive to insulin (because of its high levels in your blood) and all of these effects are the major causes of insulin resistance. So your goal should be to minimize those rapid spikes in your blood sugar levels and one way to do that is to eliminate the consumption of simple carbohydrates.
Most simple carbs in our diet come from processed and refined foods such as sugar, white flour, cakes, lollies, sweets, pasta, bread, sodas but even fruit juices. So by simply switching to more whole foods in your diet, you’ll be already making some significant improvements.
• Complex carbs & fiber
Complex carbs, on the other hand, won’t have such a drastic impact on your glucose levels. That’s because they have much more complicated structures and your body needs to break them down before they can be absorbed into your blood. This means that the increase of blood glucose levels after eating complex carbs will be much slower and steadier and your pancreas will be able to keep up.
Complex carbs are usually the ones in their original form (whole grains, whole fruit, legumes, vegetable) and they also include fiber. Fiber is also classified as a carbohydrate but our body can’t actually absorb it (most of it) because of its complicated linkages that we don’t have any enzymes for.
However, fiber is still extremely important to our health and one of its benefits is that it can slow down the absorption of sugars into our blood. So any carbs high in fiber are a much better choice if you suffer from insulin resistance.
Glycemic Index
If you want to know exactly how a certain food will react once you eat it, you can look at its Glycemic Index (GI) which measures how much and how quickly it raises your blood sugar levels. Every type of food (containing carbohydrates) will have a GI number on a scale from 1 to 100 and this number is an indicator of the food’s impact on your glucose levels.
| Number | Glycemic Index |
|---|---|
| 1-55 | low |
| 56-69 | medium |
| 70-100 | high |
The higher the number the quicker and more rapid spike in your blood sugar levels it will cause. So if you suffer from insulin resistance and PCOS, you want to consume foods that are lower on the Glycemic Index scale (low to medium).
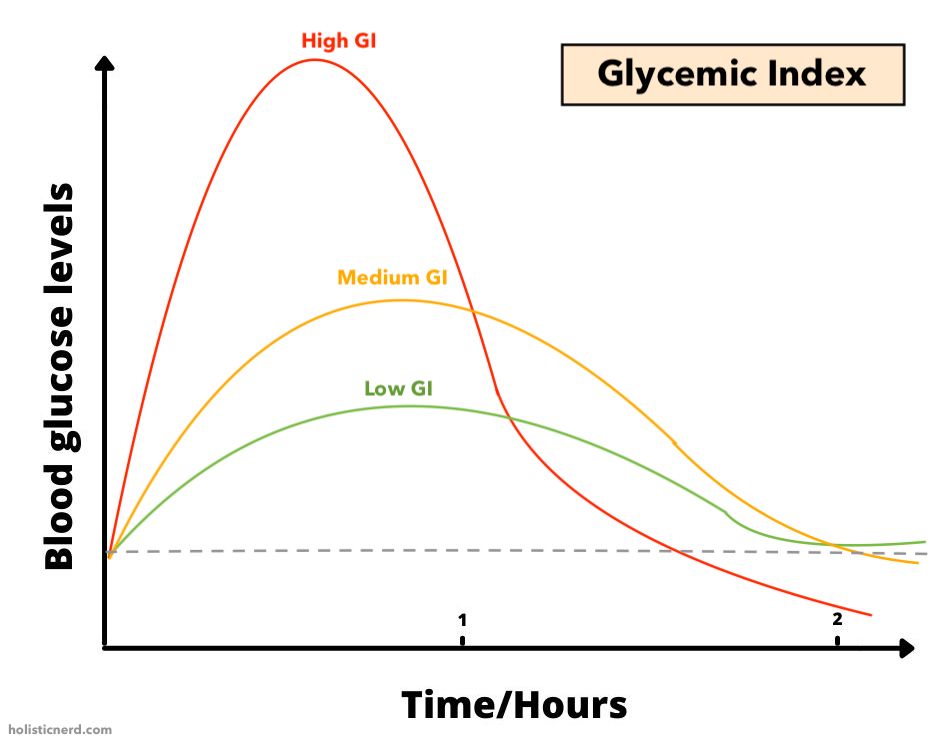
How to use glycemic index
Glycemic Index numbers can be extremely helpful for your healthy dietary choices but this method of looking at food has also its limitations you should take into account.
Unfortunately, the Glycemic Index doesn’t consider serving size and all numbers have been set by evaluating the effects of 50g of carbs in certain food compared to 50g of glucose.
This means that some types of foods, which are extremely healthy (e.g. carrots), may have a high GI number (71) but it’s very unlikely that you would consume a carrot portion consisting of 50g of carbs in one sitting.
So the effects will be actually different based on the amount you eat. If you consume 1 medium carrot (which is about 10g of carbs) your blood sugar levels won’t cause such a drastic spike.
Glycemic Load
A better way of looking at the effect that takes into account the serving size is Glycemic Load (GL). You can easily calculate it by multiplying the amount of carbs in a certain food serving (10g of carbs in 1 carrot) by the food’s GI number (71 for carrots).
So a Glycemic Load for 1 medium carrot will be actually 7.1 (10 x 0.71 = 7.1). By looking at this number, you can also consider the food low, medium, or high on the GL scale.
| Number | Glycemic Load |
|---|---|
| 1-10 | low |
| 11-19 | medium |
| 20-60 | high |
How to choose the right food
So now you see that eating one carrot has a GL number 7.1, which is considered low, so there’s no reason for not including carrots in your diet (in moderation) despite their high GI number. In general, if you eat food in its natural form (whole vegetables, fruits, grains, beans) it’s unlikely that there’ll be 50g of carbs in one portion and you’ll also benefit from its fiber and water content.
However, this is not true for processed and packaged foods (e.g. donuts, white bread, cakes, cookies) which are high in GI but also in GL because of their high sugar and low fiber content. So if you want to benefit from a low GI diet, you don’t have to restrict your veggies and fruit consumption but rather try to minimize refined and processed sources of carbohydrates.
If you’d like to get more tips on how to reverse PCOS through dietary changes, I’ve created an easy-to-follow guide accessible here: ‘The Best PCOS Diet (Ultimate Guide)’
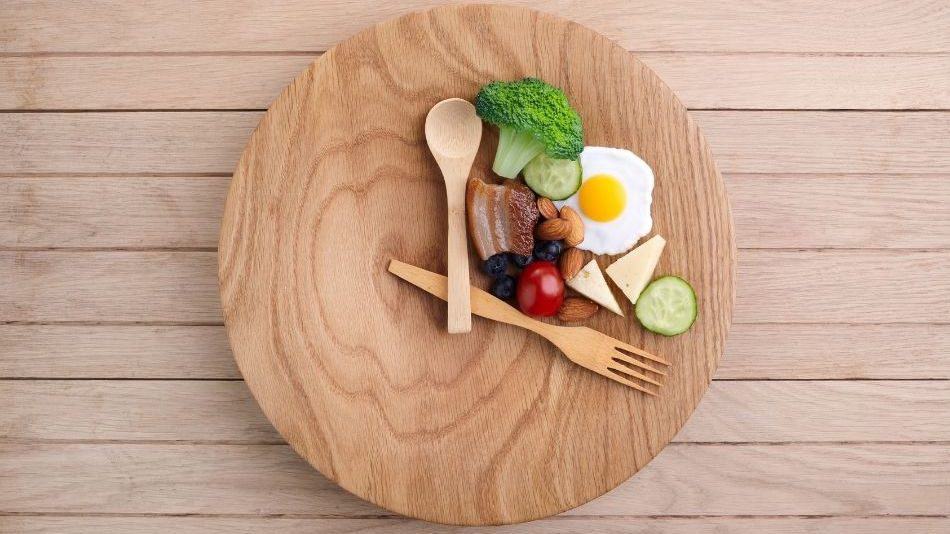
3. Intermittent Fasting
How does food frequency affect insulin resistance?
You now know that the types of food you eat directly impact your blood sugar levels, hence either increase or decrease your insulin resistance. But what about the timing of your food? Is it also important? Well, according to science yes it is!
That’s because insulin is only released when you eat (in response to glucose in your blood) so it only makes sense that the more frequently you eat the more spikes in your blood sugar levels you get, followed by insulin release.
So constantly snacking and eating 5-6 meals/day doesn’t sound like a good solution for keeping your insulin levels in check. Intermittent fasting, on the other hand, has been found to be highly effective in blood sugar regulation, improving insulin sensitivity and decreasing the risks of type 2 diabetes.
What is intermittent fasting?
Intermittent fasting has gained a lot of attention lately because of its promising health benefits. But what exactly is this popular phenomenon?
In short, intermittent fasting basically means that you only eat in a certain period of the day (e.g. from 12pm till 18pm) and the rest of the time (e.g. from 18pm till 12pm) which also include sleep, you don’t consume any food allowing your body to fast (and decrease those elevated insulin levels).
This may seem a bit extreme at first, but for some people, it can actually just mean skipping breakfast or dinner (you can set your eating window however fits you).
How does intermittent fasting help with insulin resistance?
By eating less frequently, you basically give your body a break from all those glucose and insulin spikes and it will regain its sensitivity and will respond to the hormone more effectively.
There’s a lot of good evidence supporting these beneficial effects on insulin resistance (apart from many others). But it also seems that there might be some differences between genders due to their different hormonal profiles and that women might benefit more from shorter fasts.
Intermittent fasting is also not recommended for people with a history of eating disorders and pregnant/breastfeeding women so you should always consider all of those aspects (and consult with your doctor) before trying it out.
You can learn more about intermittent fasting and its benefits and risks for PCOS here: ‘Is Intermittent Fasting Good Or Bad For PCOS & Why?‘
My experience with intermittent fasting
Based on my own experience, I do suggest you give it a try if you suffer from PCOS and insulin resistance as I got some great results from it and the evidence is now becoming even stronger. I’ve been implementing intermittent fasting since 2017 and now it’s just a normal part of my life.
You may want to start with a qualified supervisor to make sure you do it correctly and gain the most benefits. But if it’s not for you, you can also start by simply reducing your total number of meals to 3 meals/day without snacking in between.
If you suffer from constant cravings between meals (another common symptom of PCOS), implementing intermittent fasting may also benefit you. If you want to know more you can check out my article ‘PCOS Cravings: How To Reduce Appetite & Exessive Hunger‘.
4. Exercise
How does exercise affect insulin resistance?
Exercise is another lifestyle aspect that can benefit you on so many different levels if you suffer from insulin resistance. Regular exercise can definitely help you to lose weight and drastically change your body composition but exercise has also direct effects on your insulin levels and insulin sensitivity.
That’s because when you exercise your muscle cells need to take in glucose (with the help of insulin) from your blood to be used for energy so you’ll be immediately regulating your blood sugar levels and decreasing the amount of insulin in your blood.
If you repeat this process frequently (if you exercise on a regular basis) your body will become more efficient and you’ll be able to restore your insulin sensitivity.
So if you’re looking for some long-term effects, you can actually retrain your body and significantly improve your insulin resistance with exercise in the long run (with the right diet).
What is the best type of exercise for insulin resistance?
There are many different types of exercise you can include in your lifestyle and each of them has its own benefits. You can read my article ‘What Is The Best Exercise For PCOS & Why?‘ if you want to know more about the effects of different types of exercise on PCOS.
The good news is that any type of exercise will be effective in increasing your body’s insulin sensitivity so the most important question is what type of activity you’ll be able to stick to long-term. Because if you want to retrain your body to react to insulin more effectively, you’re gonna need to give it enough training.
So when it comes to exercise for insulin resistance, consistency is key! If you’re new to exercise it’s even more important to choose an activity that you genuinely enjoy and that you’ll be able to stick to.
“When it comes to exercise for insulin resistance, consistency is key!”
But on the other hand, don’t feel like you only need to do one type of training. I personally love diversity and I find that mixing it up is what keeps it most interesting, enjoyable, and beneficial for me.
5. Sleep
Why is sleep important?
It shouldn’t come as a surprise that if you want your body to function properly (including your hormones and metabolism) you need to give it enough high-quality time to recover. And that’s exactly what sleep is for!
Sleep science is very interesting because there are still so many areas unexplored and things unexplained. But the more research on sleep is done the more it is clear just how important it actually is.
There are just so many important processes that happen when you’re asleep (that you might not even realize) but without them, you wouldn’t be able to live. You can think of sleep as your body’s ultimate time for clearance, repairing, and maintenance.
During sleep, it basically puts everything back in order and recharges so you can function properly. This also includes your endocrine (hormone) system and metabolism.
How does sleep affect insulin resistance?
Many studies have shown that sleep deprivation is closely linked to diabetes and insulin resistance because of its negative effects on blood sugars and hormone regulations.
But it’s also been found that even one night of partial sleep deprivation (4h of sleep) can cause some serious metabolic disruptions and an increase in insulin resistance.
So the effects of sleep on insulin resistance are pretty drastic confirming that sleep really is precious and we should treat it that way.
“Sleep really is precious and we should treat it that way.”
Can sleep be replaced?
Unfortunately, there’s nothing you can do to replace this essential activity to gain all of its benefits and effects on health. That’s why sleep should never be compromised and you should try to make it your priority and allow your body to do its job.
You want to make sure that you reserve enough time for sleep (7-8h) every day and that it’s a high-quality time. Once you get your sleeping schedule sorted you’ll be able to see some immediate results and improvements not only in your health but also in many other life aspects.
6. Stress Management
How does stress affect insulin resistance?
Stress is another important player that can significantly contribute to insulin resistance development. That’s because when you’re stressed you have increased levels of cortisol and adrenal (the ‘stress hormones’) in your body and those hormones can actually impair your insulin functions.
Stress is a normal part of life and it’s actually critical for some situations (e.g. life or death scenarios) but it can become really problematic if you’re exposed to stressful situations too much and too often.
Studies have found that chronic stress is strongly associated with insulin resistance and the development of diabetes. So one of the ways to improve your metabolic functions and insulin sensitivity is with effective stress management.
How to reduce stress
Reducing stress in today’s busy world is an extremely challenging task to do and (in my opinion) also very individual. There are so many different factors that come to play and there is no one single recipe for stress reduction that will work for everyone.
“There is no one single recipe for stress reduction that will work for everyone.”
That’s why it’s important you put a lot of effort into finding the best way of stress management for you and don’t completely dismiss this important life aspect.
However, there is one method of stress reduction that is for everyone and that is getting enough high-quality sleep. As you now know, sufficient sleep is crucial for combating insulin resistance but it’s also closely linked to stress.
If you are sleep deprived the stress hormones (especially cortisol) in your body become elevated which will only increase your overall stress levels.
Diet and physical activity have also a direct impact on your stress levels and that’s why you should focus on making changes in all of those lifestyle areas as they all interact with each other (just like all processes in your body) and therefore they are equally important.
Resources:
- Barnosky, A. R., Hoddy, K. K., Unterman, T. G., & Varady, K. A. (2014). Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Translational research : the journal of laboratory and clinical medicine, 164(4), 302–311. https://doi.org/10.1016/j.trsl.2014.05.013
- Bergman, R.N., Kim, S.P., Catalano, K.J., Hsu, I.R., Chiu, J.D., Kabir, M., Hucking, K. and Ader, M. (2006), Why Visceral Fat is Bad: Mechanisms of the Metabolic Syndrome. Obesity, 14: 16S-19S. https://doi.org/10.1038/oby.2006.277
- Brouns, F., Bjorck, I., Frayn, K. N., Gibbs, A. L., Lang, V., Slama, G., & Wolever, T. M. (2005). Glycaemic index methodology. Nutrition research reviews, 18(1), 145–171. https://doi.org/10.1079/NRR2005100
- Centres For Disease Control & Prevention (2019) Research Behind the National DPP Available at: https://www.cdc.gov/diabetes/prevention/research-behind-ndpp.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Fprevention%2Fprediabetes-type2%2Fpreventing.html
- Donga, E., van Dijk, M., van Dijk, J. G., Biermasz, N. R., Lammers, G. J., van Kralingen, K. W., Corssmit, E. P., & Romijn, J. A. (2010). A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. The Journal of clinical endocrinology and metabolism, 95(6), 2963–2968. https://doi.org/10.1210/jc.2009-2430
- Eriksson, J., Taimela, S., & Koivisto, V. A. (1997). Exercise and the metabolic syndrome. Diabetologia, 40(2), 125–135. https://doi.org/10.1007/s001250050653
- Gołąbek, K. D., & Regulska-Ilow, B. (2019). Dietary support in insulin resistance: An overview of current scientific reports. Advances in clinical and experimental medicine : official organ Wroclaw Medical University, 28(11), 1577–1585. https://doi.org/10.17219/acem/109976
- Lizneva, D., Suturina, L., Walker, W., Brakta, S., Gavrilova-Jordan, L., & Azziz, R. (2016). Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertility and sterility, 106(1), 6–15. https://doi.org/10.1016/j.fertnstert.2016.05.003
- Lunger, F., Wildt, L., Seeber, B. (2013) Accurate screening for insulin resistance in PCOS women using fasting insulin concentrations. Gynecol Endocrinol.;29(6):541-4. https://doi.org/10.3109/09513590.2013.774362
- Mattson, M. P., Longo, V. D., & Harvie, M. (2017). Impact of intermittent fasting on health and disease processes. Ageing research reviews, 39, 46–58. https://doi.org/10.1016/j.arr.2016.10.005
- Moghetti P. (2016) Insulin Resistance and Polycystic Ovary Syndrome. Curr Pharm Des.;22(36):5526-5534. https://doi.org/10.2174/1381612822666160720155855
- Norman, R. J., Davies, M. J., Lord, J., & Moran, L. J. (2002). The role of lifestyle modification in polycystic ovary syndrome. Trends in endocrinology and metabolism: TEM, 13(6), 251–257. https://doi.org/10.1016/s1043-2760(02)00612-4
- Papalou, O., & Diamanti-Kandarakis, E. (2017). The role of stress in PCOS. Expert review of endocrinology & metabolism, 12(1), 87–95. https://doi.org/10.1080/17446651.2017.1266250
- Washington University School of Medicine. (2007, November 7). Fat Cells Send Message That Aids Insulin Secretion. ScienceDaily. Retrieved May 6, 2021 from www.sciencedaily.com/releases/2007/11/071106133108.htm
- Weickert, M. O., & Pfeiffer, A. F. (2008). Metabolic effects of dietary fiber consumption and prevention of diabetes. The Journal of nutrition, 138(3), 439–442. https://doi.org/10.1093/jn/138.3.439
- Yan, Y. X., Xiao, H. B., Wang, S. S., Zhao, J., He, Y., Wang, W., & Dong, J. (2016). Investigation of the Relationship Between Chronic Stress and Insulin Resistance in a Chinese Population. Journal of epidemiology, 26(7), 355–360. https://doi.org/10.2188/jea.JE20150183